NOS News•today, 6:00 PM
-
Sander Zurhake
healthcare editor
-
Judith Pennarts
Investigative editorial team Nieuwsuur
-
Sander Zurhake
healthcare editor
-

Judith Pennarts
Investigative editorial team Nieuwsuur
Hospital care in the Netherlands is in danger of coming to a standstill in the coming years, because there are more and more patients with multiple diseases at the same time. Inadequate cooperation between medical specialists, the rapid aging of the population and the complex financing of the healthcare system reinforce this trend.
Doctors are now working on solutions, but their implementation faces bureaucratic obstacles. The impasse leads to fragmented care and can cause disasters, for example due to medication errors.
This is evident from an inventory by the joint investigative editors of the NOS and News hourwho spoke to seven scientific professional associations of medical specialists, doctors and professors.
The The conclusion is that the demographic change in the population up to and including 2040 will lead to an overwhelming of the current hospital system. Today, 5.7 million people already have two or more chronic conditions. By 2040 there will be 6.6 million, says the Scientific Council for Government Policy.
The majority of those patients will turn to hospitals. This often concerns elderly people who have multiple diseases at the same time. Not yet published figures from the Northwest Hospital Group in Alkmaar, which the research group saw, confirm the growing demand that patients with multiple diseases place on healthcare capacity.

From previous research by NOS and News hour it has already become clear that healthcare is in danger of structurally coming to a standstill because patients end up unnecessarily in hospital. The research editors have now investigated whether hospitals can handle the expected influx of patients with multiple diseases who do belong in the hospital. The system also appears to be no longer equipped for this.
“Care is now focused on the treatment of one specific disease,” says professor of internal medicine Barbara van Munster. “And the specialist is trained to provide that treatment as best as possible.”
The general practitioner treats a large number of conditions, but people end up in hospital for several conditions
According to Van Munster, the financing of healthcare maintains this working method. The system is set up to fund treatments for one disease such as cancer, where ‘multidisciplinary consultations’ are funded, but not for patients with multiple conditions.
This is a ticking time bomb regarding the accessibility of hospital care. Because it is precisely these patients who will become the most common hospital patients in the coming years. “The GP treats a large number of conditions,” says Van Munster. “But if one has multiple conditions, and I mean three, four, five, then they end up in the hospital.”
Attack on hospital capacity
At the Northwest Hospital Group in Alkmaar, physician-researcher Ursula de Ruijter has provided insight into how much of a burden such a type of patient places on the total capacity of a hospital. Of the 140,000 patients who visited an outpatient clinic in Alkmaar in 2019, only a quarter of them had multiple diseases at the same time. But almost half of all consultations went to this group. According to Professor Van Munster, this case is representative for the rest of the Netherlands.
In this video Ursula de Ruijter shows how much capacity is needed for one patient with multiple conditions.
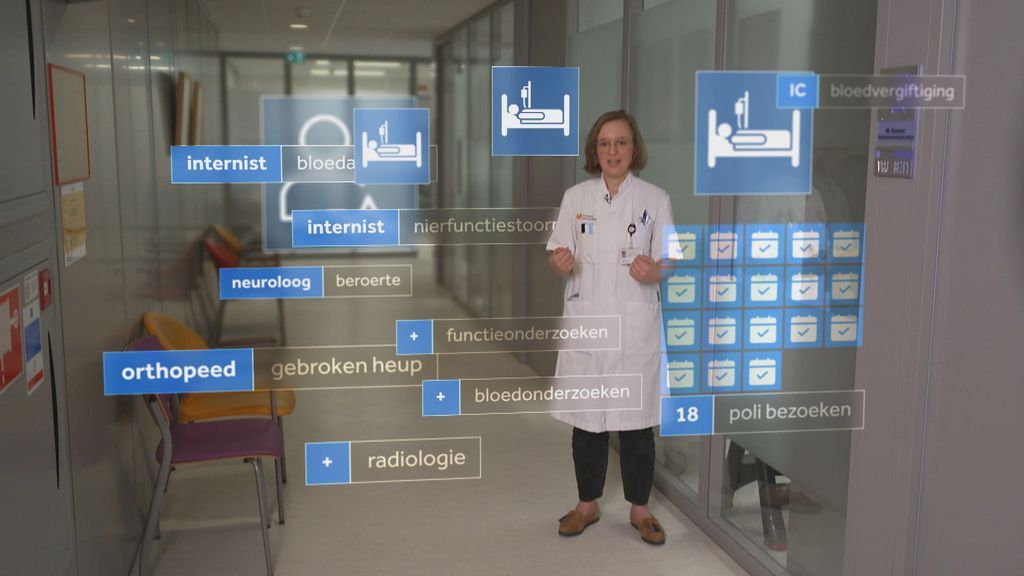
Ursula’s very elderly patient became entangled in a web of specialists
Examples of collaboration between doctors for patients with multiple problems are few, but do exist. At the Jeroen Bosch Hospital in Den Bosch, internists, clinical geriatricians, pulmonologists, cardiologists and hospital doctors jointly create a treatment plan for complex patients in a special department every morning.
There are also financing problems here, but these have been temporarily resolved because the departments of these medical specialists have taken part of their budget have submitted. This allowed specifically trained hospital doctors to get to work to examine patients more broadly and to supervise daily consultations between specialists.
Successful alternative
Clinical geriatrician Esther Cornegé shows a scientific publication with the results. “The length of stay is two days shorter and patient satisfaction is also very good. In addition, patients visit fewer doctors because the collaboration has halved the number of mutual referrals.”
You notice in everything that current thinking is still very disease-oriented.
However, implementing this program nationally is proving difficult. In her role as chair of the professional association for clinical geriatricians, Cornegé experiences a lot of reluctance from healthcare administrators and health insurers. Financially it is considered risky.
Not only financing is an obstacle. “You notice in everything that current thinking is still very disease-oriented, with insufficient attention to the fact that an increasing part of the population has more than one disease,” says Robin Peeters, head of internal medicine at Erasmus MC and also an advocate. of cooperation.
This blind spot is also visible in the Integrated Care Agreement, essentially the blueprint for how future Dutch healthcare should be organized. But the patients suffering from multiple diseases are mentioned only three times. Agreements about better cooperation between medical specialists are not an issue.
We cannot afford to wait until we have the numbers.
As chairman of the Dutch Internists Association, Peeters experiences how a lack of attention hinders support. For five years he has been trying to arrange financing with the Dutch Healthcare Authority and Zorgverzekeraars Nederland (ZN) to achieve better cooperation between medical specialists. Without reimbursements, consultations cannot be financially viable for hospitals.
Wasted time
Before insurers reimburse such consultations, they want to see in black and white that the discussions are useful. Peeters wants to set up pilots for this, but he experiences little willingness to help from health insurers. They contradict this and argue that it is up to Peeters to come up with a concrete research plan. “We have not yet received this plan.”
“We are all wasting valuable time this way,” says Peeters. “A fully developed business case is a utopia at this stage.” Because of the impending healthcare crisis, he emphasizes the urgency to test now what works and what does not. “We really have to tackle this together now. The healthcare system is almost bursting at the seams, so we cannot afford to wait until we have the numbers.”









